A recent study has found that caffeine might exacerbate the negative effects of chronic sleep restriction on the brain’s grey matter. The researchers discovered that people who consumed caffeine during a period of sleep restriction showed more significant reductions in grey matter volume compared to those who did not consume caffeine. The findings were recently published in Scientific Reports.
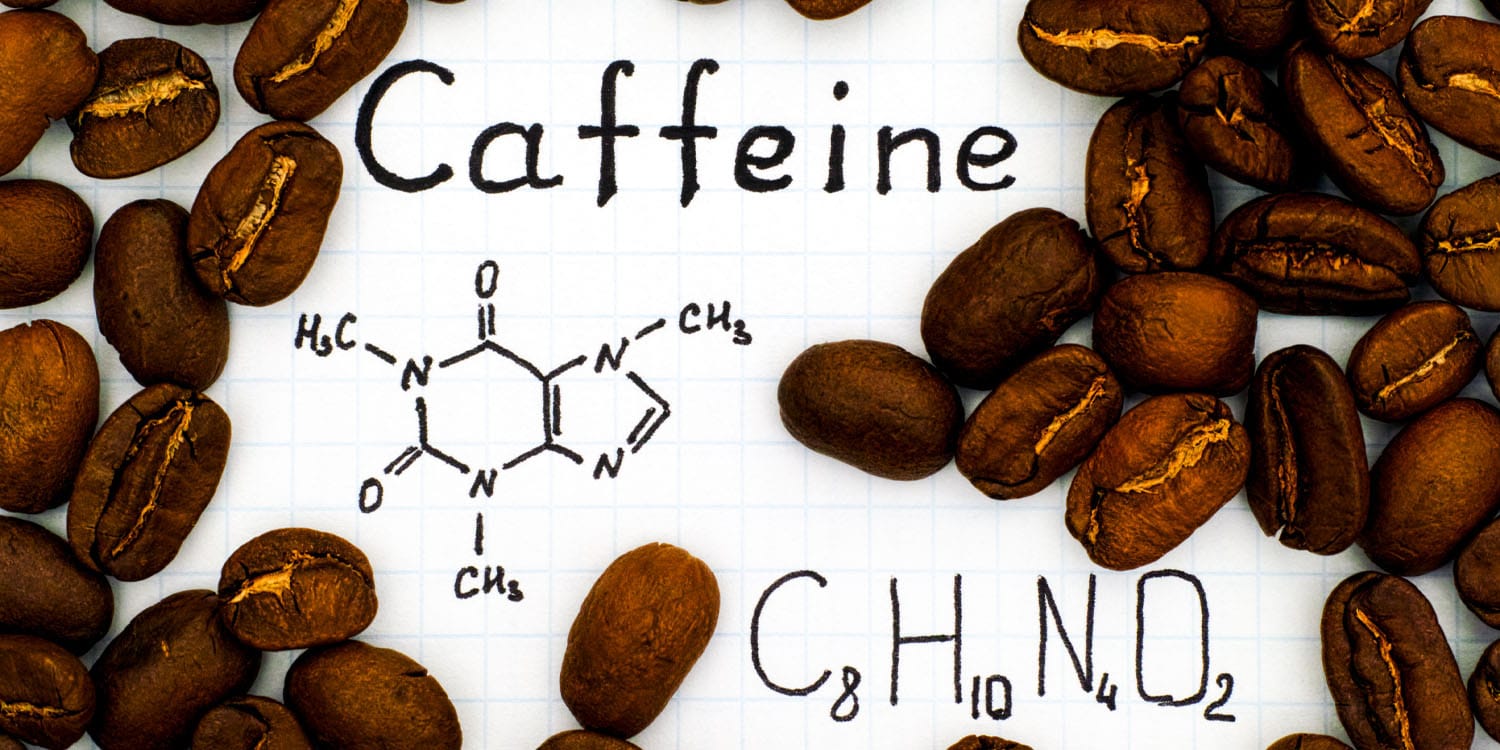
Caffeine is the most widely used psychoactive substance globally, renowned for its ability to improve alertness and alleviate cognitive impairments caused by lack of sleep. However, both acute sleep loss and daily caffeine intake have been associated with reductions in gray matter volume, a key component of the brain involved in processing information and regulating various cognitive functions.
By examining the interaction between chronic sleep restriction and daily caffeine intake, the researchers aimed to uncover whether caffeine consumption during periods of sleep deprivation would lead to further reductions in gray matter volume. Additionally, the study sought to explore the role of the adenosine system, particularly the availability of adenosine A1 receptors, in mediating the brain’s response to caffeine and sleep loss.
Adenosine A1 receptors are a type of receptor in the brain that plays a crucial role in regulating neural activity and promoting sleep. They are part of the adenosine system, which helps to balance energy consumption and maintain homeostasis. Caffeine acts as an antagonist to these receptors, blocking their action and thereby enhancing alertness and counteracting sleepiness.
The research was conducted, in part, by first author Yu-Shiuan Lin of the University Psychiatric Clinics Basel in Switzerland and senior author David Elmenhorst of the Institute of Neuroscience and Medicine at Forschungszentrum Jülich in Germany.
“The conception of this work was inspired by the findings in Dr. Yu-Shiuan Lin’s previous study at the Centre for Chronobiology. There we observed a caffeine concentration-dependent decrease in gray matter after a controlled 10-day caffeine intake, which was independent of the caffeine-induced vasoconstriction and was only partially mitigated after 36 hours,” the two researchers told PsyPost in a joint statement.
“This effect of caffeine on gray matter plasticity added up to the abundant animal evidence that demonstrates the involvement of adenosine receptors, the primary property caffeine binds to and exerts effects through, in modulating the synaptic plasticity in central nervous systems. To understand a potential role of adenosine in gray matter plasticity, Yu-Shiuan reached out to Professor David Elmenhorst at the Forschungszentrum Jülich for this collaborative project.”
“At the time David, was conducting a PET-MRI study together with the German Aerospace Center to investigate the effects of chronic sleep restriction and daily caffeine intake on adenosine A1 receptor (A1R) availability. Besides the A1R measurement in vivo, this study was exhilarating as it could potentially provide insights to the adenosinergic modulation in brain plasticity through the interference with sleep.”
“The metabolism and signaling of adenosine play a crucial role in the homeostatic mechanism of sleep,” Lin and Elmenhorst explained. “Disrupted sleep can in turn alter adenosine signaling and has been frequently found to impair brain structures in both animal models and humans. Insufficient sleep also consolidates the caffeine intake behaviors, and both are, often concurrently, prevalent in the modern society.
“Hence, we took the opportunity and repurposed the PET and T1-weighted MR images in addition to the data of Arterial Spin Labeling to account for the caffeine effects on brain perfusion, and examined the gray matter plasticity after chronic sleep restriction with and without combining use of caffeine, as well as the potential mediation of A1R in these gray matter responses.”
The study was conducted at the German Aerospace Center’s research facility in Cologne with 36 healthy adult participants, including 15 females and 21 males, aged around 29 years. These participants were selected based on their low habitual caffeine intake (less than 450 mg per day) and non-smoking status. The participants were divided into two groups: one group received caffeine-containing coffee (the CAFF group), while the other received decaffeinated coffee (the DECAF group).
The experiment spanned nine days in a controlled laboratory setting. It started with an adaptation day, followed by two baseline days where participants had 8 hours of sleep per night. This was followed by five days of chronic sleep restriction, with participants limited to 5 hours of sleep per night, and concluded with a recovery day of 8 hours of sleep. During the chronic sleep restriction phase, the CAFF group received 200 mg of caffeine in the morning and 100 mg in the afternoon, while the DECAF group received equivalent volumes of decaffeinated coffee.
To measure the effects on gray matter volume, participants underwent magnetic resonance imaging (MRI) scans and positron emission tomography (PET) scans at three points: after the baseline days, after the chronic sleep restriction phase, and after the recovery day. Saliva samples were collected regularly to monitor caffeine levels, ensuring accurate tracking of caffeine intake and its physiological effects.
The results of the study indicated that chronic sleep restriction led to changes in gray matter volume, which were significantly influenced by caffeine intake. Participants who did not consume caffeine (DECAF group) during the sleep restriction phase showed an increase in gray matter volume in several brain regions, including the prefrontal cortex, temporal-occipital cortex, and thalamus. These regions are associated with various cognitive and sensory functions, indicating a potential compensatory response to sleep loss.
“It was somewhat surprising to us to observe an increase, instead of a decrease in gray matter in the participants without caffeine (DECAF group) after chronic sleep restriction,” Lin and Elmenhorst told PsyPost. “However, an earlier study (Dai et al. (2018)) shed light on a potential explanation to this finding. This study examined the changes in gray matter along the course between 20 and 36 hours of wakefulness, and they found that multiple brain regions in fact started from showing an increase in the early stage (20h) and turned to be a reduction later (36h).”
“Although the impact of a total sleep deprivation could not be generalized to chronic sleep restriction, we speculated that the gray matter responses to an increasing duration and/or intensity of sleep loss may not follow a linear trajectory. More studies are certainly warranted to systematically examine the gray matter changes in different patterns of sleep restrictions.”
In contrast, participants who consumed caffeine (CAFF group) during the sleep restriction phase exhibited a decrease in gray matter volume in these same regions. This suggests that caffeine might inhibit the brain’s compensatory mechanisms during periods of insufficient sleep, potentially exacerbating the negative impact of sleep loss on brain structure.
The researchers also found that individual differences in adenosine receptor availability played a significant role in the extent of gray matter changes. The participants with lower baseline availability of subcortical adenosine receptors experienced greater reductions in gray matter volume when they consumed caffeine during sleep restriction. This finding highlights the importance of adenosine receptor activity in mediating the effects of sleep deprivation and caffeine on brain structure.
“People who have a higher A1R availability seem to have more resistance to the effect of caffeine on gray matter,” the researchers explained. “After a recovery sleep and around 30-hour caffeine withdrawal, most of the changes in gray matter have recovered, except the increased dorsolateral prefrontal cortex associated with chronic sleep restriction and the decreased thalamus associated caffeine intake,”
“It is commonly known that caffeine intake combats sleepiness. Our data further indicate that caffeine intake also interferes with the brain plasticity induced by sleep loss. However, caffeine does not simply suppress or normalize the gray matter change but also impacts gray matter in an opposite direction. It is unclear how the effect of this brain plasticity manifests on the cognitive behavioral levels; what we know is that it is likely demonstrating the adenosine modulation in neural homeostasis.”
Despite its rigorous methodology, the study has some limitations to consider. The sample size was relatively small, and participants were selected based on specific genetic profiles related to caffeine metabolism, which might limit how well the findings apply to the broader population.
Additionally, while MRI scans showed changes in grey matter, they can’t tell us exactly what caused these changes. It could be a gain or loss of neurons, changes in synapse density, or variations in the number of support cells like microglia. To pinpoint these specific changes, future studies could use PET scans with special markers to measure synapses, mitochondria, or microglia, the researchers explained.
“The synaptic homeostasis hypothesis (SHY) states that ‘sleep is the price we pay for brain plasticity,’” the researchers said. “A decade has passed since SHY was published, and this fascinating hypothesis is still yet to be tested in humans in vivo. David therefore has been dedicated to studying the molecular mechanism of sleep-wake regulations using biomedical imaging. On the other hand, Yu-Shiuan continues focusing on pharmacological PET-MR imaging to investigate the adenosinergic modulation and its role in the effects of caffeine. We are hoping that future outcomes along these lines will provide insights to the findings in this current work.”
The study, “Repeated caffeine intake suppresses cerebral grey matter responses to chronic sleep restriction in an A1 adenosine receptor-dependent manner: a double-blind randomized controlled study with PET-MRI,” was authored by Yu-Shiuan Lin, Denise Lange, Diego Manuel Baur, Anna Foerges, Congying Chu, Changhong Li, Eva-Maria Elmenhorst, Bernd Neumaier, Andreas Bauer, Daniel Aeschbach, Hans-Peter Landolt, and David Elmenhorst.