A recent study published in Brain
challenges long-held assumptions about Alzheimer’s disease treatment. Researchers at the University of Cincinnati found that new monoclonal antibody drugs may slow cognitive decline by increasing levels of a critical brain protein called amyloid-beta 42 (Aβ42), rather than simply reducing amyloid plaques in the brain. This discovery shifts the focus from plaque buildup to the potential role of Aβ42 in maintaining brain health.
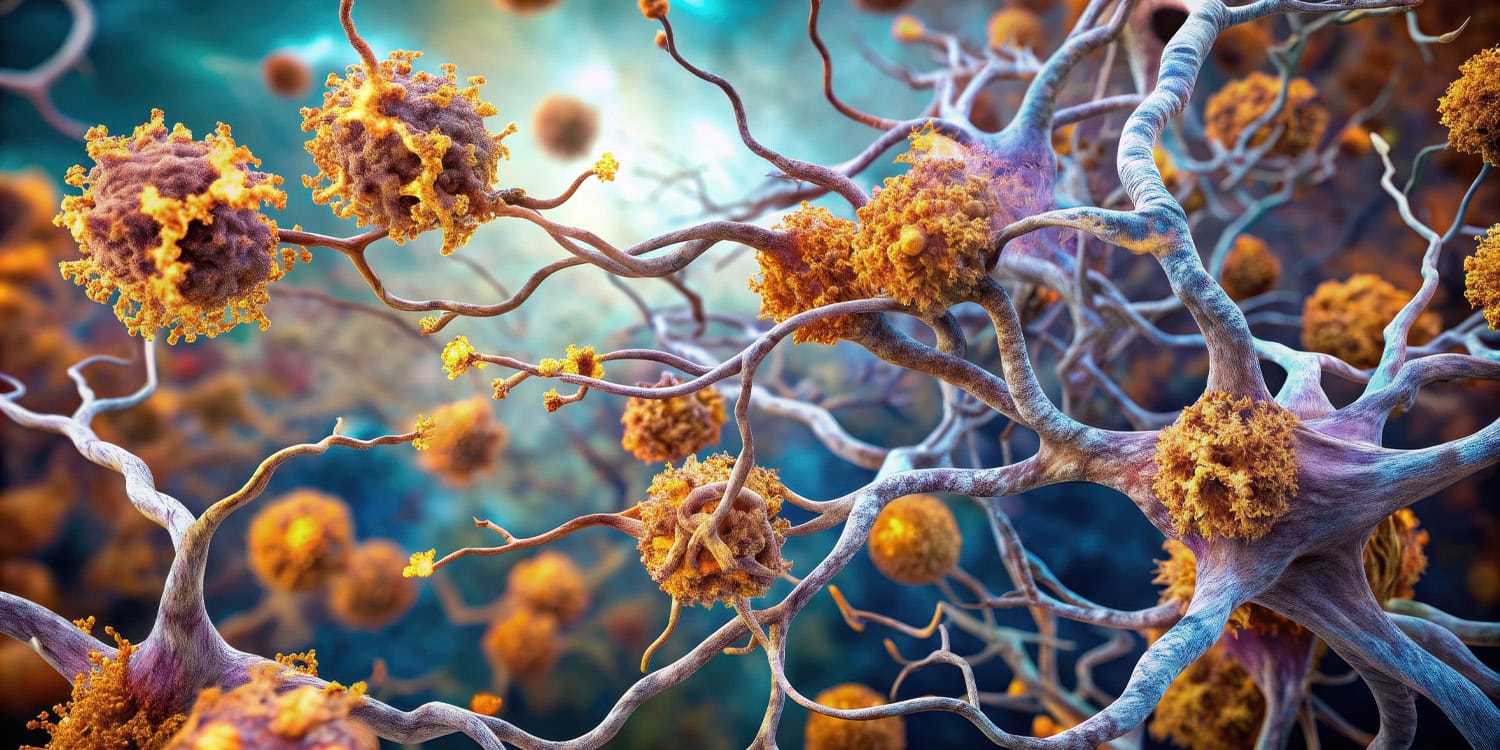
Alzheimer’s disease is the most common form of dementia, characterized by progressive memory loss, cognitive decline, and changes in behavior. The condition gradually impairs daily functioning and quality of life, affecting millions of people worldwide. At a biological level, Alzheimer’s is marked by two main features: the buildup of amyloid plaques outside neurons and neurofibrillary tangles of tau protein inside neurons.
Amyloid-beta is a protein fragment naturally produced in the brain during normal cell processes. It exists in several forms, but two variants, Aβ40 and Aβ42, are of particular interest in Alzheimer’s research. Aβ40 is the more common form, comprising about 90% of all amyloid-beta produced and considered relatively benign under normal conditions. Aβ42, although less abundant, is more prone to clumping and forming plaques. This increased aggregation potential has made Aβ42 the focus of theories about Alzheimer’s pathology.
The amyloid cascade hypothesis, first proposed in the early 1990s, has dominated the field for decades. According to this theory, Alzheimer’s begins when Aβ42 molecules stick together to form clumps called oligomers. These oligomers aggregate into amyloid plaques, which are thought to disrupt neuronal communication, trigger inflammation, and eventually lead to the widespread damage seen in Alzheimer’s. Support for this hypothesis came from genetic studies showing that mutations in genes affecting amyloid production are linked to rare, inherited forms of Alzheimer’s.
Despite the appeal of the amyloid cascade hypothesis, efforts to treat Alzheimer’s by removing amyloid plaques have largely failed. Over 30 clinical trials targeting amyloid have either shown no significant cognitive benefits or, in some cases, worsened symptoms. This has led researchers to question whether plaques are the root cause of Alzheimer’s or a secondary byproduct of the disease. Observations that many older individuals with plaques never develop dementia have further fueled this debate.
Neurology professor Alberto J. Espay and his team hypothesized that the loss of normal, soluble Aβ42 in the brain, rather than the buildup of plaques, might drive Alzheimer’s pathology. Research supporting this idea suggests that Aβ42 plays a critical role in maintaining neuronal health and synaptic function. Its depletion, not its aggregation, may be what leads to cognitive decline.
The researchers also noted that some newly approved monoclonal antibody treatments (aducanumab, lecanemab, and donanemab) unintentionally increased Aβ42 levels in cerebrospinal fluid, which correlated with cognitive improvements. These findings prompted the team to investigate whether raising Aβ42 levels might explain the benefits of these treatments, offering a fresh perspective on the disease’s underlying mechanisms.
“Most anti-Aβ interventions had succeeded in clearing the brain from amyloid plaques, yet they were either futile or statistically favored the placebo group,” explained Espay, the director and endowed chair of the Gardner Family Center for Parkinson’s Disease and Movement Disorders and co-author of Brain Fables, the Hidden History of Neurodegenerative Diseases and a Blueprint to Conquer Them.
“I was interested in finding out what made aducanumab, lecanemab, and donanemab special. Along the way, I learned that along with removing amyloid, virtually all monoclonal anti-Aβ antibodies also increase Aβ42 in cerebrospinal fluid.”
“I was interested in finding out whether one could explain the cognitive outcomes from the opposite end of protein homeostasis—by the increases in Aβ42. This is at the core of the two opposing hypotheses in neurodegeneration in general and Alzheimer’s disease in particular: one posits that the disease is caused by the accumulation of amyloid plaques (so-called amyloid cascade hypothesis); the other that the disease is caused by the loss of Aβ42 as it transforms into amyloid plaques (the proteinopenia hypothesis). I have reviewed data in favor of the latter.”
In their new study, Espay and his colleagues analyzed data from 24 randomized clinical trials of monoclonal antibody drugs designed to target amyloid plaques. These trials included nearly 26,000 patients diagnosed with early or moderate Alzheimer’s disease. The researchers focused on changes in two key biomarkers: amyloid plaque levels (measured through imaging) and cerebrospinal fluid levels of Aβ42. They also examined cognitive performance using standardized tests like the Alzheimer’s Disease Assessment Scale and the Clinical Dementia Rating.
The team used statistical methods to compare the cognitive outcomes of patients treated with monoclonal antibodies against changes in amyloid plaques and Aβ42 levels. By evaluating the relationship between these biomarkers and cognitive improvement, the researchers aimed to determine which factor was more closely linked to slowing cognitive decline.
The results showed that increases in Aβ42 levels were just as strongly associated with cognitive improvement as the reduction of amyloid plaques. In fact, drugs that raised Aβ42 levels showed a consistent correlation with better cognitive outcomes. Conversely, treatments that lowered Aβ42 levels—such as certain enzyme inhibitors—worsened cognitive performance.
The researchers proposed that amyloid plaques might not directly cause Alzheimer’s symptoms. Instead, plaques could represent a protective response by the brain to stress or injury. The real issue, they suggested, might be the depletion of soluble Aβ42, which plays a critical role in neuron health and synaptic function. When Aβ42 levels drop below a critical threshold, cognitive decline appears to accelerate.
The findings highlight that “there are two sides to any story,” Espay told PsyPost. “We have thought that the only explanation for any potential benefit of the newly approved monoclonal antibodies for Alzheimer’s is that they are good at removing amyloid plaques from the brain. Yet many other interventions have done that in the past, to no avail. The alternative explanation for any benefit is the increase in the levels of Aβ42 in cerebrospinal fluid, which most antibodies accomplish (remarkably, such data is mostly confined to the supplementary materials of the trial reports).”
But the study, like all research, has limitations. The researchers relied on aggregated data from clinical trials, which may limit the precision of their analyses. “We don’t have individual-level data, as these are not shared by the companies that own the data. This meant we worked with lowered power to find significant differences,” Espay explained.
In other words, the researchers had to base their conclusions on group-level trends rather than detailed, individualized information. This limitation reduces the ability to account for variations in how different patients respond to treatments, potentially obscuring important nuances that could refine their findings or reveal more precise relationships between biomarkers and cognitive outcomes.
The study also raises practical challenges. Monoclonal antibody treatments, while effective at increasing Aβ42 levels, carry risks, including brain inflammation and shrinkage. Looking forward, Espay hopes “to test the potential benefits of directly increasing Aβ42 without the toxicities imposed upon the brain by removing amyloid (quite a toxic enterprise).”
“There is resistance to looking at Alzheimer’s as a loss, which is paradoxical,” he added. “We have long become too comfortable with the idea that Alzheimer’s is about a ‘gain’—of the amyloid plaques. But in fact, amyloid forms as a reaction to many things. And if too much of it is necessary in such a reaction, less of the normal protein from which it comes (Aβ42) remains.”
The study, “Increases in amyloid-β42 slow cognitive and clinical decline in Alzheimer’s disease trials,” was authored by Jesus Abanto, Alok K. Dwivedi, Bruno P. Imbimbo, and Alberto J. Espay.