A study of healthy volunteers in the United Kingdom found that the administration of escitalopram, a common antidepressant, increases activity in the right amygdala region of the brain during an emotional processing task known to activate this area. This change in activity was not accompanied by a change in mood. The research was published in the Journal of Psychopharmacology.
Escitalopram is a selective serotonin reuptake inhibitor (SSRI) commonly prescribed to treat depression and generalized anxiety disorder. It works by increasing levels of serotonin, a neurotransmitter in the brain that plays a key role in mood regulation. Escitalopram effectively improves mood, energy levels, and overall well-being by restoring the balance of serotonin.
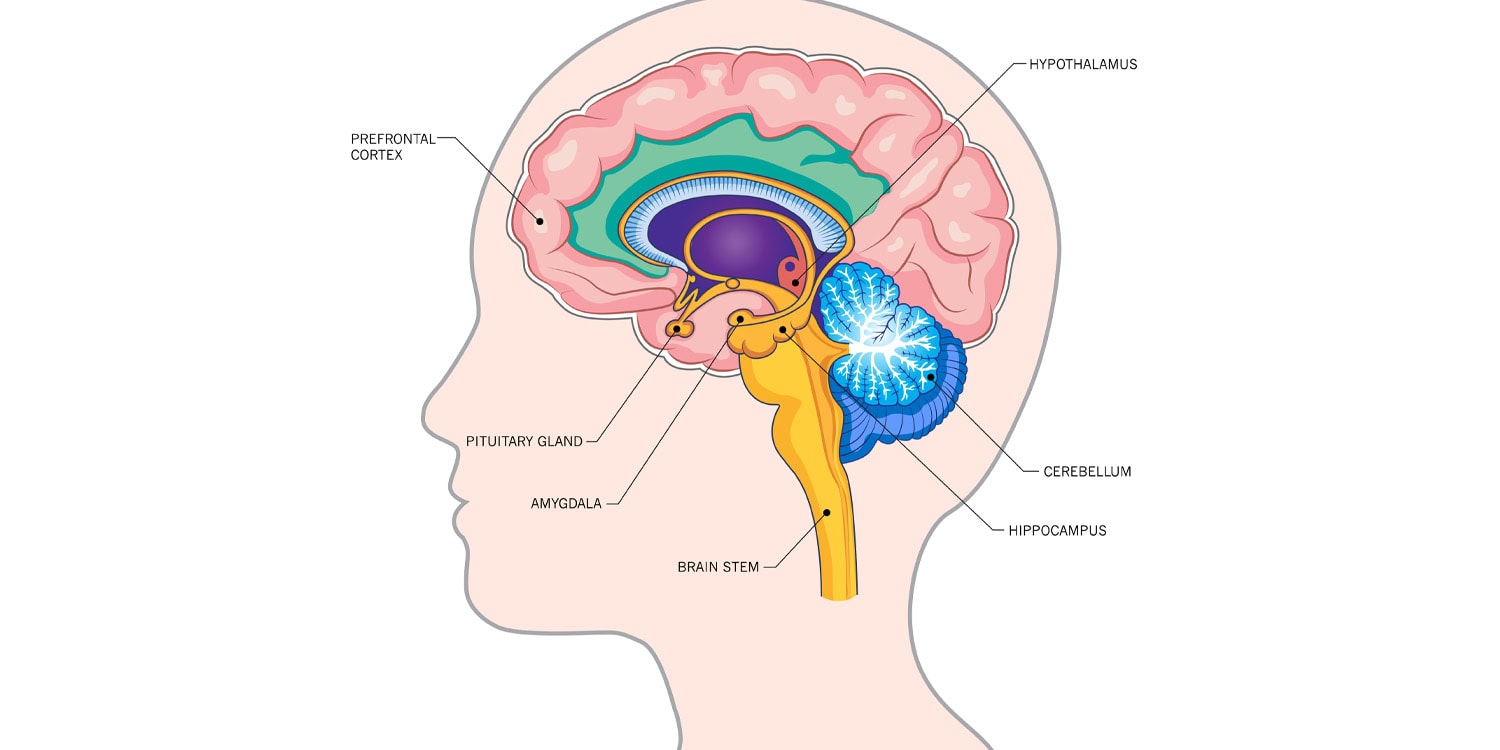
However, serotonin is involved not only in mood regulation but also in various brain functions, including cognition and chronic pain management. Many of these functions are associated with neural structures in the prefrontal cortex and the amygdala, yet there is little research on escitalopram’s effects on these areas outside of its impact on mood.
Study author Paulina B. Lukow and her colleagues sought to investigate whether escitalopram affects activation and connectivity in the prefrontal cortex and amygdala during an emotional face-processing task. Their hypothesis was that this drug would reduce activity in the amygdala region and decrease its connectivity with other brain areas. They also anticipated increased activity in the subgenual anterior cingulate cortex, a part of the prefrontal cortex involved in regulating mood, processing emotions, and responding to stress.
Study participants were 98 healthy volunteers recruited through public advertisements. They were between 18 and 50 years of age and in good mental health.
Participants visited the lab on three occasions. During the first visit, they completed several assessments for depression and anxiety. At the second visit, they performed an emotional face-processing task while undergoing functional magnetic resonance imaging (fMRI). In the task, participants viewed pictures of faces displaying various emotions and were asked to indicate the gender of each face. Previous studies have shown that this task activates parts of the brain involved in emotional processing, including the amygdala region.
After this session, participants were randomly assigned to receive either 10 mg of escitalopram or a placebo (an identical-looking tablet without the active substance) for the next 12-23 days. Participants were unaware of whether they were taking escitalopram or the placebo. After the administration period, they underwent another fMRI scan.
The results showed that, prior to treatment, the emotion-processing task led to increased activation in the amygdala and several other brain regions. When comparing the two treatment groups after the escitalopram/placebo period, researchers found that participants treated with escitalopram had higher activity in the right amygdala region. There were no differences in activity in other brain regions.
This change in amygdala activity was not accompanied by a change in mood. There were also no differences between groups in connectivity of the studied brain regions.
“We found evidence that escitalopram treatment of just over 2 weeks in healthy volunteers may selectively increase right amygdala activation during emotional face processing, but not its connectivity with the dorsomedial cortex,” the study authors concluded.
The study sheds light on the effects of escitalopram on neural activity in the part of the brain responsible for processing emotions. However, it remains unclear whether these differences in neural activity translate into observable differences in psychological functioning.
The paper, “Amygdala activity after subchronic escitalopram administration in healthy volunteers: A pharmaco-functional magnetic resonance imaging study,” was authored by Paulina B Lukow, Millie Lowther, Alexandra C Pike, Yumeya Yamamori, Alice V Chavanne, Siobhan Gormley, Jessica Aylward, Tayla McCloud, Talya Goble, Julia Rodriguez-Sanchez, Ella W Tuominen, Sarah K Buehler, Peter Kirk, and Oliver J Robinson.