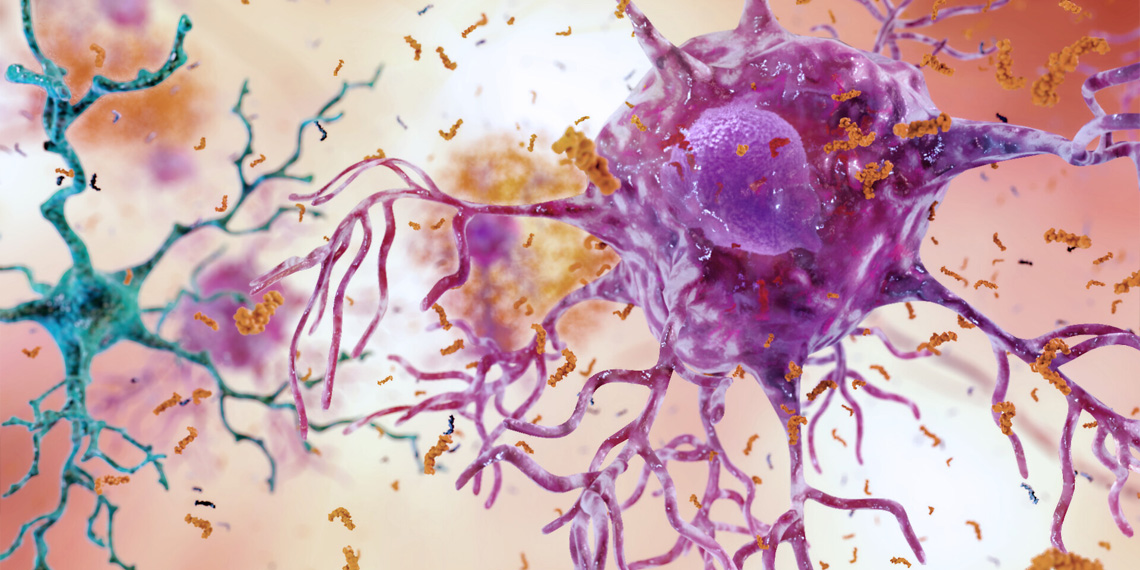
A new study published in Alzheimer’s & Dementia has found that while Alzheimer’s disease is more common in women, men tend to experience a quicker decline in brain health and cognitive abilities once the disease process begins. Researchers discovered that in the years following the initial buildup of amyloid plaques – a hallmark of Alzheimer’s – men showed more rapid increases in key markers of brain damage and faster decreases in brain volume and cognitive performance compared to women. These findings suggest that sex plays a significant role in how Alzheimer’s disease progresses after the earliest biological changes occur in the brain.
Although previous studies have shown that more women than men are diagnosed with dementia, there has been less focus on whether the underlying biological changes and symptoms progress differently by sex. By following a group of older adults over time, the research team hoped to shed light on the pattern of changes in the blood and brain that occur after amyloid-β buildup starts, and to determine if these changes are influenced by a person’s sex. Their aim was to learn more about how the disease unfolds during its early and middle stages, which could help guide future treatments and improve our understanding of the disease’s natural history.
“We know there is a difference in the prevalence in dementia between men and women. However, it is not known whether the rate of disease progression differs based on sex. This is important because it could affect treatment approaches and prognosis,” said study author Keenan Walker, a tenure-track investigator at the National Institute on Aging.
The research team used data collected over many years from the Baltimore Longitudinal Study of Aging. This study has been tracking a community of older adults since 1958, with regular visits that include various tests and brain scans. For the current research, the investigators focused on participants who had evidence of amyloid-β accumulation in the brain, as determined by positron emission tomography scans. From this group, they identified 78 participants who had at least one PET scan showing amyloid buildup. The study included 45 men and 33 women.
Once a participant’s scan showed signs of amyloid-β, the researchers estimated the age when this buildup first began. They then compared how blood-based markers, brain volumes measured by magnetic resonance imaging scans, and results of cognitive tests changed in the years after that estimated start of amyloid buildup.
The study uncovered a significant difference in the progression of Alzheimer’s disease between men and women after the initial buildup of amyloid plaques in the brain. Specifically, in the years following the estimated onset of amyloid accumulation, men showed faster increases in blood markers associated with Alzheimer’s pathology (phosphorylated tau) and nerve cell damage (neurofilament light).
These biological changes were mirrored in brain structure and cognitive function. Brain scans revealed that men experienced more rapid brain shrinkage and a quicker progression toward an Alzheimer’s-like pattern of brain atrophy. Cognitively, men demonstrated faster declines in certain abilities, particularly those related to visual-spatial skills and executive functions like planning and decision-making. Although not definitive, the study also hinted that men might progress to diagnosable cognitive impairment and dementia in a shorter timeframe after amyloid onset compared to women.
“Amyloid plaque deposits on the brain is a core feature of Alzheimer’s disease that occurs very early in the disease process,” Walker told PsyPost. “After amyloid plaques accumulate, other components of the Alzheimer’s disease process that are more closely associated with cognitive function, such as tau pathology and neuron damage, begin to emerge.
“We found that after amyloid plaques accumulate, men have an accelerated disease trajectory (as defined by tau pathology and neuron damage), compared to women. This is what blood biomarker data suggests. These finding of steeper declines after amyloid plaque deposition were also supported by neuroimaging and cognitive measures. In summary, although the prevalence of Alzheimer’s dementia tend to be higher in women, the rate of disease progression is faster in men.”
Like all research, there are limitations. The sample size was relatively small, and the participants were primarily white and highly educated, which may limit how broadly the findings can be applied to other populations. “Our findings were only observed in a single cohort,” Walker noted. “Replication in an independent cohort is needed to confirm the results.”
Future research might also explore the biological or environmental reasons why men seem to experience faster changes after amyloid buildup compared to women. Understanding these reasons could lead to more effective, personalized treatments for Alzheimer’s disease.
The study, “Sex differences in the trajectories of plasma biomarkers, brain atrophy, and cognitive decline relative to amyloid onset,” was authored by Cassandra M. Joynes, Murat Bilgel, Yang An, Abhay R. Moghekar, Nicholas J. Ashton, Przemysław R. Kac, Thomas K. Karikari, Kaj Blennow, Henrik Zetterberg, Madhav Thambisetty, Luigi Ferrucci, Susan M. Resnick, and Keenan A. Walker.