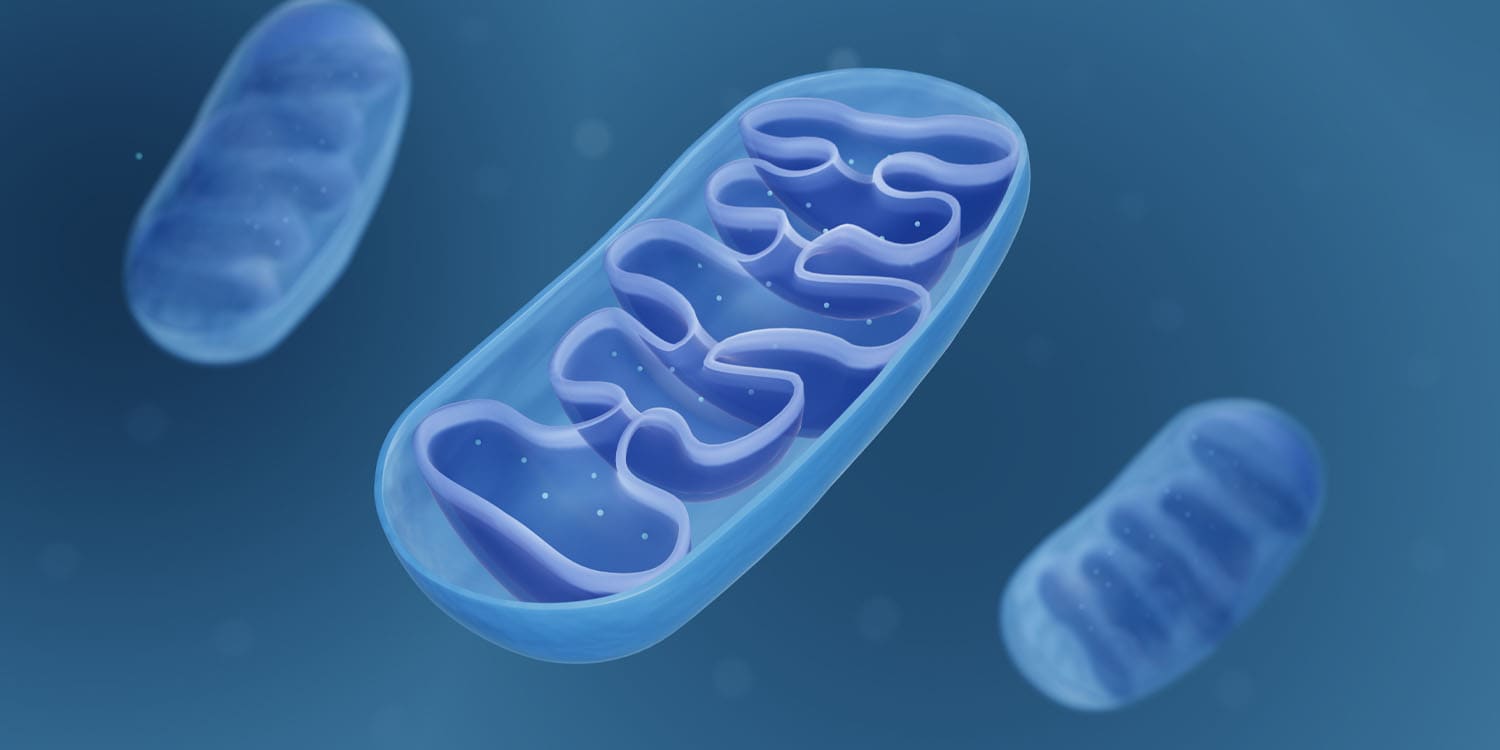
A new study by researchers at Columbia University sheds light on how our experiences and emotions might influence brain health. The study provides evidence that mitochondria, the tiny powerhouses inside our brain cells, could be the key players in this relationship. In older adults, positive psychosocial experiences — such as a larger social network or a greater sense of purpose — are linked to healthier brain mitochondria. Conversely, negative experiences — like social isolation or depression — are associated with less robust mitochondrial function.
The findings have been published in the Proceedings of the National Academy of Sciences (PNAS).
“How the mind shapes our biology, potential for health, and risk of disease is perhaps the biggest gap in medicine. We know from decades of research, and from our personal experiences, that how we feel influences our health. But there is little science on this,” said study author Martin Picard, an associate professor and endowed chair in energy and health.
“Mitochondria are the energy and information processor of each cell. They keep us alive and well, and enable each cells in our body and brain to communicate with each other and to act as an integrated whole – to be in health. We need to uncover the psychobiological connections linking what we experience to the biology of energy. This is the focus of mitochondrial psychobiology, and of this study by Dr. Caroline Trumpff.”
To better understand the role of mitochondria, the researchers used data from two long-term studies involving nearly 450 older adults in the United States. These participants had provided detailed information about their psychosocial experiences over two decades and had agreed to donate their brains for postmortem analysis.
The researchers aimed to quantify both positive and negative psychosocial experiences. They created indices that combined various psychosocial factors into overall positive and negative scores. Positive factors included a larger social network, greater social activity, a strong sense of purpose, and overall well-being.
Negative factors encompassed social isolation, depressive symptoms, negative mood, and perceived stress. By converting these reports into standardized scores, the researchers could systematically compare the participants’ psychosocial experiences with the biological state of their brain mitochondria.
For the biological analysis, the researchers focused on the dorsolateral prefrontal cortex, a brain region involved in executive functions and emotional regulation. They measured the abundance of mitochondrial proteins in this area using sophisticated proteomic techniques. Instead of analyzing thousands of individual mitochondrial genes, they grouped related genes into seven categories, or “mitotypes,” which reflect different aspects of mitochondrial function. This innovative approach allowed for a more interpretable and statistically robust analysis of mitochondrial health.
The findings revealed a clear association between psychosocial experiences and mitochondrial protein abundance. Participants with higher positive psychosocial scores had greater levels of mitochondrial proteins, particularly those involved in oxidative phosphorylation (OxPhos), a key process for cellular energy production. In contrast, those with higher negative psychosocial scores had lower levels of these proteins.
“We’re showing that older individuals’ state of mind is linked to the biology of their brain mitochondria, which is the first time that subjective psychosocial experiences have been related to brain biology,” explained Trumpff, an assistant professor of medical psychology.
“In our lives we are exposed to positive and negative psychosocial factors, some of which we can nourish and develop,” Picard told PsyPost. “These factors, we now learn in Dr. Trumpff’s study, are linked to the biology of the energy transformation centers in our brains – the mitochondria. We have long known that things like exercise, fasting, and low carb diets can stimulate mitochondria. This study brings subjective experiences – that stuff that makes us human – in the mix of things that may influence energy flow in our brains.”
A key finding of the study was that psychosocial experiences accounted for 18 to 25% of the variance in the abundance of complex I proteins. Complex I is the largest and most upstream enzyme in the OxPhos pathway. This significant percentage indicates that a considerable portion of the differences in mitochondrial function among individuals can be attributed to their psychosocial experiences. Positive psychosocial factors were linked to higher levels of proteins involved in energy transformation, while negative factors were associated with lower levels of these proteins.
The researchers were surprised by the strength of the effects. “The psycho-biological correlation of 18-25% is remarkable compared to other similar studies,” Picard said.
Interestingly, the findings also suggested that glial cells and neurons might respond to or even contribute to psychosocial experiences in opposite ways. Glial cells, which include astrocytes, microglia, and oligodendrocytes, were found to have higher mitochondrial gene expression associated with positive psychosocial experiences. This means that individuals who reported more positive experiences had glial cells with more active mitochondrial functions.
In contrast, the same positive experiences were linked to lower mitochondrial gene expression in neurons. This divergence indicates that while glial cells might enhance their energy production and other mitochondrial functions in response to positive experiences, neurons might reduce these activities.
Glial cells play supportive roles in the brain, such as providing nutrients to neurons, maintaining homeostasis, and participating in immune responses. Their increased mitochondrial activity in response to positive experiences could enhance these supportive functions, potentially leading to better overall brain health. On the other hand, neurons, which are primarily responsible for transmitting information throughout the brain, might reduce mitochondrial activity as a way to optimize energy use or reduce oxidative stress under positive psychosocial conditions.
These results were consistent across various subgroups, including different genders and cognitive statuses, indicating a broad and robust connection between psychosocial experiences and mitochondrial health. But as with all research, there are some caveats to consider. One major limitation is the reliance on postmortem brain samples.
“We obviously had to ask people how they felt before they died, and had to wait for them to die to analyze their mitochondria postmortem,” Picard noted. “So there is a time gap between the psychosocial assessment and the biological measures.”
Developing non-invasive techniques to measure mitochondrial health in living individuals could significantly advance this field of research. Such methods would enable continuous monitoring of mitochondrial function, allowing for early detection of potential issues and timely interventions. Researchers are already exploring ways to assess mitochondrial health in clinical settings, which could revolutionize how we monitor and promote brain health.
“Our long-term goals are to create a science of health and healing that integrates the science of energy with the human experience of energy,” Picard said. “This will help us bring the mind into medicine, and create a more holistic framework to help each person reach their optimal state of health.”
The study, “Psychosocial experiences are associated with human brain mitochondrial biology,” was authored by Caroline Trumpff, Anna S. Monzel, Carmen Sandi, Vilas Menon, Hans-Ulrich Klein, Masashi Fujita, Annie Lee, Vladislav A. Petyuk, Cheyenne Hurst, Duc M. Duong, Nicholas T. Seyfried, Aliza P. Wingo, Thomas S. Wingo, Yanling Wang, Madhav Thambisetty, Luigi Ferrucci, David A. Bennett, Philip L. De Jager, and Martin Picard.