A recent study in Nature Neuroscience provides new insights into how amyloid-beta and tau proteins, which accumulate in the brains of individuals with Alzheimer’s disease, alter brain activity and potentially contribute to cognitive decline. Researchers observed a progression from hyperactivity to hypoactivity in brain regions affected by these proteins, a shift that correlated with declines in attention and memory. These findings suggest that changes in brain activity might serve as early indicators of the disease.
Alzheimer’s disease is a progressive neurodegenerative disorder and the most common cause of dementia, affecting millions of people worldwide. It typically begins with memory loss and difficulties in thinking and reasoning, progressing in advanced stages to impairments in basic daily tasks.
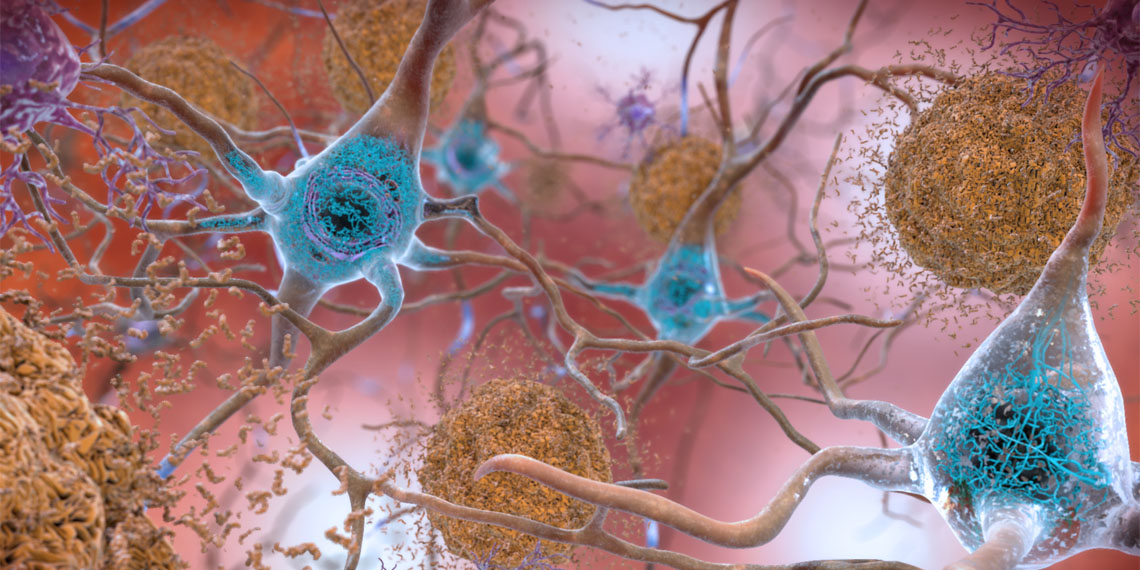
The condition is marked by the abnormal buildup of two proteins in the brain: amyloid-beta and tau. Amyloid-beta forms sticky plaques between brain cells, while tau aggregates into tangles within cells, disrupting their function. Together, these proteins are believed to drive a cascade of harmful processes, including inflammation, loss of synaptic connections, neuronal death, and ultimately brain atrophy.
Amyloid-beta and tau accumulate long before noticeable symptoms of Alzheimer’s disease appear, sometimes decades earlier. Amyloid-beta plaques often develop first, starting in high-activity brain regions like the precuneus and spreading outward. Tau tangles typically emerge later, affecting memory-critical areas such as the entorhinal cortex. Although these proteins are strongly linked to Alzheimer’s, the precise ways in which they interact to cause cognitive decline remain unclear. One leading hypothesis suggests that amyloid-beta triggers hyperactivity in brain cells, which exacerbates tau pathology and leads to progressively slower brain activity as the disease advances.
The new study aimed to fill gaps in understanding how amyloid-beta and tau disrupt brain function in humans, particularly before cognitive symptoms arise. While animal studies and computational models have suggested similar patterns, evidence of these protein-induced brain activity changes in humans was lacking.
“Alzheimer’s disease is a growing global challenge, but its progression often begins silently, years before symptoms like memory loss appear. We wanted to explore how the earliest brain changes, specifically those related to either amyloid-beta, tau protein accumulation or both, might influence brain activity and predict cognitive decline,” said study author Sylvain Baillet, a professor of neurology & neurosurgery and computer science at McGill University.
“Our goal was to contribute to the understanding of how these proteins interact with brain activity and how they affect brain function in asymptomatic individuals at risk of developing Alzheimer’s disease, ultimately seeking early markers for detection and intervention and monitoring—a question with significant repercussions beyond a fundamental understanding of disease mechanisms, as treatments are starting to become available to patients and require a delivery as early as possible and clinical monitoring.”
For their study, the researchers recruited 104 participants who were cognitively normal but had a family history of Alzheimer’s disease, placing them at an elevated risk for the condition. The researchers aimed to explore how the accumulation of amyloid-beta and tau proteins in the brain affects neural activity before the onset of symptoms. To achieve this, they used a combination of advanced imaging techniques and cognitive assessments.
Positron emission tomography (PET) scans were performed to detect and measure the presence of amyloid-beta and tau proteins in the participants’ brains. This imaging technique allowed the researchers to pinpoint specific regions where the proteins were accumulating. Magnetoencephalography (MEG), a method that measures real-time brain activity, was used to examine the neural activity patterns in these protein-rich regions. MEG is particularly effective for capturing the frequencies of brain waves, providing insights into how neural activity changes in response to protein buildup.
The researchers observed distinct patterns in brain activity linked to the presence of these proteins. Areas with high levels of amyloid-beta exhibited increased fast-frequency brain activity and reduced slow-frequency activity, reflecting a state of hyperactivity. However, when both amyloid-beta and tau were present, the activity in these regions shifted to a hypoactive state, characterized by a slowing of brain activity. This transition from hyperactivity to hypoactivity aligns with the idea that the proteins interact synergistically to disrupt normal brain function.
“The main takeaway is that subtle changes in brain activity, linked to amyloid-beta and tau protein buildup, occur long before noticeable symptoms of Alzheimer’s disease,” Baillet told PsyPost. “These changes differ depending on whether only amyloid-beta starts accumulating (yielding acceleration of brain activity), or whether the tau protein also adds to amyloid-beta accumulations (yielding considerable slowing of brain activity).”
Importantly, these participants were still asymptomatic, meaning their cognitive decline was detectable only through careful testing and not evident in everyday life. “This suggests that brain activity could serve as an early warning system for Alzheimer’s, opening up possibilities for earlier interventions to slow or prevent progression,” Baillet said.
The findings also revealed that these changes in brain activity were associated with declines in cognitive performance. Participants with more pronounced slowing of brain activity in regions affected by amyloid-beta and tau scored worse on tests of attention and memory.
“We were surprised by the extent to which changes in brain activity, particularly the transition from acceleration to slowing, predicted future cognitive decline,” Baillet explained. “Additionally, the synergistic effect of amyloid-beta and tau was striking—it was not just the presence of these proteins but how they interacted to influence brain function that mattered most. This finding underscores facets of Alzheimer’s disease that were not fully studied so far and highlights the importance of looking at brain activity in addition to measures of proteins in the brain or changes in brain structure, which occur later in the disease.”
As with all research, there are limitations. The data were collected at a single point in time, making it difficult to determine the causal relationship between protein buildup, brain activity changes, and cognitive decline. “Further research is needed to determine the underlying mechanisms,” Baillet said. “For instance is it neural acceleration for unknown causes that triggers the accumulation of amyloid-beta, or vice-versa?”
The researchers plan to address these limitations in a follow-up study by rescreening the same participants over time. Longitudinal data will help clarify how brain activity evolves as the disease progresses and whether these changes reliably predict future cognitive decline. Exploring other markers, such as blood-based measures of amyloid and tau, could also enhance the ability to detect Alzheimer’s at its earliest stages.
“Our long-term goal is to develop non-invasive tests for early detection and risk prediction in Alzheimer’s disease,” Baillet said. “We aim to refine our ability to predict disease onset, severity and cognitive decline by combining brain activity measurements with possibly other biomarkers, such as amyloid and tau from imaging or blood tests. Ultimately, we hope this research will lead to a better understanding of the actual causes of the disease, for earlier and better interventions that slow or prevent Alzheimer’s, long before symptoms appear.”
“I’d like to thank the participants in our study and my co-authors. This work would not have been possible without their trust and commitment. I’d also emphasize the importance of open science—our dataset will be made available to other researchers, ensuring that these findings can be replicated and further advanced.”
The study, “Synergistic association of Aβ and tau pathology with cortical neurophysiology and cognitive decline in asymptomatic older adults,” was authored by Jonathan Gallego-Rudolf, Alex I. Wiesman, Alexa Pichet Binette, Sylvia Villeneuve, Sylvain Baillet, and the PREVENT-AD Research Group.