Researchers have discovered that our desire for dessert, even when full, is controlled by the brain. The same brain cells that tell us we are full after a meal also trigger our craving for sugary treats afterwards, according to new research published in the journal Science. This finding reveals a specific brain circuit that drives our appetite for sugar even when our bodies don’t need more calories.
It’s a common experience: feeling completely full after a meal, yet still having room for dessert. Researchers were curious about the biological reasons behind this so-called “dessert stomach” phenomenon. They wanted to understand why we specifically crave sugary foods even when our bodies have had enough to eat. Previous research had shown that brain pathways related to reward play a role in our food choices, but the specific mechanisms that make us want sugar after feeling full were not known.
“It was previously unknown which mechanisms drive the specific appetite for high-sugar foods, particularly in states of satiety, which would explain why we eat dessert. This was what led us to start our investigations,” explained Henning Fenselau, an independent research group leader at the Max Planck Institute for Metabolism Research.
To investigate this, the researchers conducted a series of experiments primarily using mice. First, they developed a “dessert” scenario for the mice. The mice were fasted overnight and then given regular food for 90 minutes, mimicking a meal. After this “meal,” they were offered either more regular food or a high-sugar diet for 30 minutes. This allowed the researchers to study sugar intake in mice that were already full, simulating the human experience of eating dessert after a meal. They carefully measured how much of each type of food the mice ate during this “dessert period.”
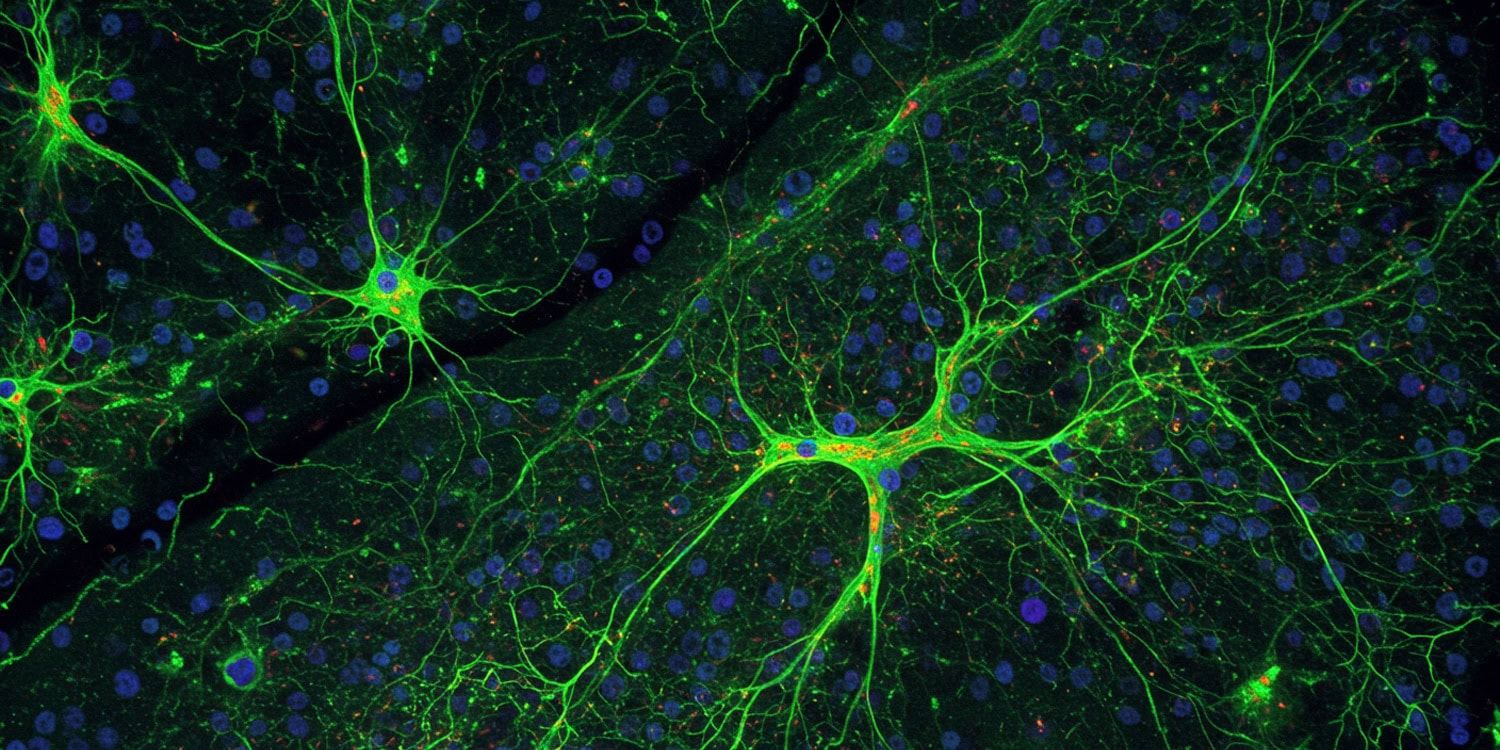
To understand the brain activity involved, the scientists focused on specific brain cells called pro-opiomelanocortin neurons, often referred to as POMC neurons, located in a brain region called the hypothalamus, which is known to regulate hunger and fullness. POMC neurons are considered master regulators of satiety (the feeling of being full and satisfied after eating). These neurons are normally activated when we’ve eaten enough food, and they play a key role in telling us to stop eating. They achieve this by releasing specific signaling molecules, including one called alpha-melanocyte-stimulating hormone. This hormone acts on other brain areas to decrease appetite and food intake, helping to maintain a stable body weight.
To explore this unexpected function, the researchers used advanced techniques to monitor and manipulate these neurons in the mice. To begin, the research team designed a “dessert” scenario for mice to mimic human eating habits. They fasted mice overnight and then gave them access to regular food for 90 minutes, simulating a meal. Following this, they offered the mice either more regular food or a high-sugar diet for 30 minutes, representing the “dessert period.” By measuring the amount of food consumed during this dessert period, they found that mice, even when full from their initial meal, ate significantly more of the high-sugar diet compared to regular food. This established that mice, like humans, exhibit a preference for sweet foods even in a state of fullness.
To investigate the role of POMC neurons in this sugar preference, the scientists used optogenetics and chemogenetics, techniques that allow for precise control of neuronal activity. Using optogenetics, they genetically modified POMC neurons in mice to be activated or inhibited by light. With chemogenetics, they used a drug to selectively inhibit or activate POMC neurons. When they used these techniques to inhibit POMC neurons or specifically the projections of POMC neurons to the paraventricular thalamus (PVT) – another brain region – in sated mice, they observed a significant reduction in the consumption of high-sugar food during the dessert period. This indicated that POMC neurons, specifically their activity in the pathway to the PVT, are necessary for driving sugar appetite in states of fullness.
To understand when and how POMC neurons become active, the researchers used fiber photometry, a technique to measure the real-time activity of neurons in living mice. They inserted a tiny optical fiber into the PVT region of mice and used a fluorescent sensor to detect the activity of POMC neuron terminals – the parts of the neurons that release signaling molecules – in this area. They monitored this activity while mice were presented with and consumed sugary food. The measurements revealed a strong and rapid increase in the activity of POMC neuron terminals in the PVT specifically when the mice were given access to the high-sugar diet.
Interestingly, this activity increase occurred not only when the mice were eating the sugar but also when they were presented with cues that predicted sugar, such as a specific smell they had learned to associate with sugar. Furthermore, even when mice tasted sugar for the first time, the POMC-to-PVT pathway was activated. This suggests that this brain pathway is involved in both the anticipation and consumption of sugar, and that the response to sugar is, at least in part, innate.
To determine if activating the POMC-to-PVT pathway was enough to create a preference for sugar, the researchers used a conditioned flavor preference test combined with optogenetics. They allowed mice to choose between two flavored diets and then, using optogenetics, activated the POMC-to-PVT pathway whenever the mice ate the less preferred flavor. They found that activating this pathway while eating a specific flavor was sufficient to make the mice develop a strong preference for that flavor, shifting their preference towards what was initially the less appealing option.
However, when they tested if activating this pathway created a general sense of reward or pleasure, using tests for place preference and real-time place preference, they found no evidence that it did. This indicated that the POMC-to-PVT pathway is specifically involved in creating a preference for sugar-associated flavors, rather than a general reward signal.
To investigate if similar brain mechanisms are at play in humans, the researchers conducted functional magnetic resonance imaging (fMRI) studies. They scanned the brains of human volunteers while the participants consumed a sugary solution compared to water. The fMRI results showed that, similar to what was observed in mice, the activity in the PVT region of the human brain decreased in response to sugar consumption. This finding supports the idea that the POMC-to-PVT pathway and its role in sugar appetite may be conserved across species, suggesting that the “dessert stomach” phenomenon has similar underlying brain mechanisms in both mice and humans.
Finally, the researchers wanted to know if this POMC-to-PVT pathway was specific to sugar, or if it was also involved in the appetite for other palatable foods, like fat. They compared the activity of the POMC-to-PVT pathway in mice when they consumed either high-sugar or high-fat diets. They found that while both types of diets increased activity in the pathway, the response to sugar was significantly stronger than the response to fat.
When they manipulated the POMC-to-PVT pathway, they found that it specifically affected sugar intake but had little impact on the consumption of high-fat food. This suggests that the POMC-to-PVT opioid pathway is particularly specialized for regulating the appetite for sugar, distinct from the mechanisms that drive appetite for other types of palatable foods like fat.
“Our data show that the brain’s principal regulator of satiety – POMC neurons – not only promote satiety signaling, but also switch on the specific appetite for sugar when our body has enough energy,” Fenselau told PsyPost. “They mediate this newly-identified function by releasing the endogenous opioid beta-endorphin.”
Further research could explore the long-term effects of chronic activation of this pathway by high-sugar diets, and how this might contribute to the development of compulsive eating behaviors or metabolic disorders.
“We are interested to determine how our findings could be applied to combat obesity and excessive sugar consumption,” Fenselau said. “There are already opioid receptor blockers (combined with other receptor antagonist) that are FDA-approved drugs for obesity treatment. We think that using and tailoring them more specifically could give new ideas how to combat obesity, particularly in subjects that consume high levels of sugar.”
The study, “Thalamic opioids from POMC satiety neurons switch on sugar appetite,” was authored by Marielle Minère, Hannah Wilhelms, Bojana Kuzmanovic, Sofia Lundh, Debora Fusca,
Alina Claßen, Stav Shtiglitz, Yael Prilutski, Itay Talpir, Lin Tian, Brigitte Kieffer, Jon Davis, Peter Kloppenburg, Marc Tittgemeyer, Yoav Livneh, and Henning Fenselau.