A new study published in the Journal of Affective Disorders shows that individuals with depression exhibit slower and less variable activity in the part of the brain responsible for processing what we see. Researchers found that the visual area at the back of the brain does not mirror the overall activity of the brain as strongly as it does in healthy individuals, and that this sluggishness is linked with both the severity of depressive symptoms and the slowing of physical movements.
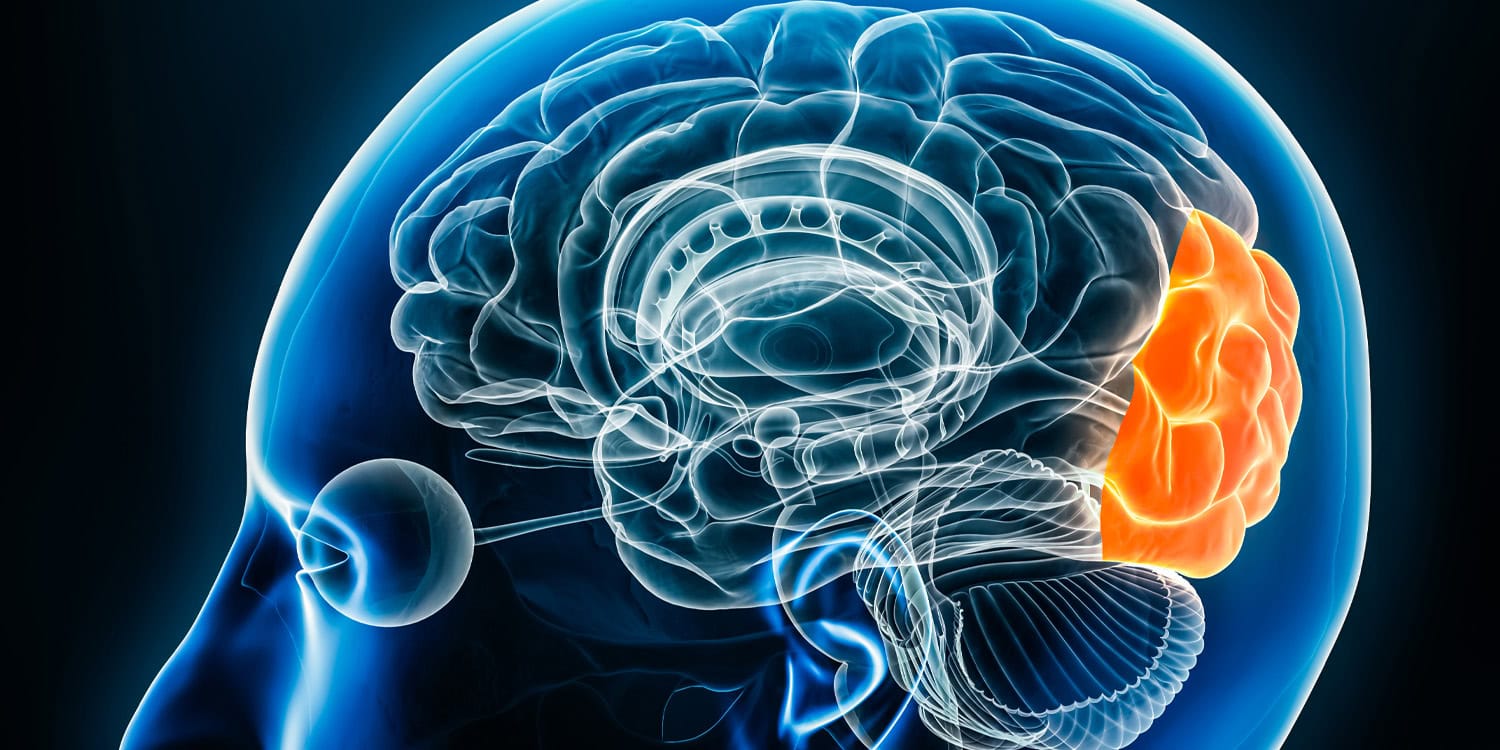
Major depressive disorder is a complex condition characterized by a range of symptoms, including changes in mood, cognition, social interaction, and movement. While visual perception changes, like experiencing the world in “slow motion” or as “gray-colored,” are often reported by people with depression, this aspect has received less attention in research. Prior studies have demonstrated physical and chemical changes in the occipital cortex of individuals with depression, and even suggest that stimulating this brain area with magnetic pulses can have antidepressant effects.
However, the timing of these neural activity changes – how the brain’s visual center changes its activity over time – remained unclear. Therefore, the researchers aimed to investigate the dynamic features of spontaneous brain activity in the occipital cortex, and to determine how it relates to depressive symptoms, especially psychomotor retardation (slowed movements and speech).
“Depressed patients are often very slow in their behavior and psychomotor activity,” said study author Georg Northoff, a professor at the University of Ottawa Institute of Mental Health Research and author of Neurowaves: Brain, Time, and Consciousness. “We therefore ask the following question: Is a primary sensory region like the visual cortex, where all environmental objects and events are processed, abnormally slow in its neural activity in depression? And does that relate to the depressive symptoms?”
To investigate this, the researchers used a technique called resting-state functional magnetic resonance imaging, or fMRI. This method allows scientists to measure brain activity indirectly by detecting changes in blood flow while a person is simply resting quietly in the scanner, not performing any specific task. The study involved 49 participants diagnosed with major depressive disorder and 50 healthy control participants with no history of mental illness. The individuals with depression were all inpatients at a mood disorders unit and were experiencing an acute depressive episode.
All participants underwent a thorough clinical assessment by psychiatrists to confirm diagnoses and rule out other medical or psychiatric conditions. The severity of depressive symptoms in the patient group was measured using the Hamilton Depression Rating Scale, a standard questionnaire used to quantify depression. Importantly, the researchers also specifically assessed psychomotor retardation using a subset of items from this scale that reflect slowed movements and thinking.
The researchers focused their analysis on the visual cortex, specifically examining both the primary visual cortex (V1), which is involved in basic visual processing, and a higher-order visual area called hMT+, known for its role in processing motion.
The core of the analysis involved several key measures. First, the researchers calculated what is known as global signal correlation. This technique assesses how much the activity in a specific brain region, in this case, the visual cortex, reflects the overall activity of the entire brain. A high global signal correlation means that the region’s activity is closely synchronized with the global brain activity, while a low correlation suggests it is more independent.
Second, they examined the functional connectivity of the visual cortex. This measures how strongly the activity in the visual cortex is related to the activity in other brain regions, such as areas in the prefrontal cortex (involved in higher-level thinking) and subcortical regions like the thalamus and hippocampus (involved in emotion and memory), which are known to be affected in depression. They looked at these connections for the visual cortex as a whole, as well as for the specific regions V1 and hMT+.
Finally, to get at the dynamics or speed of brain activity, the researchers used a measure called median frequency. This measure essentially summarizes the dominant frequency of brain activity within a region. A lower median frequency indicates that slower brain activity patterns are more prominent, while a higher frequency suggests faster activity. They calculated the median frequency in the visual cortex and then examined whether this measure was related to the severity of depression symptoms in the patient group. They also analyzed the brain activity in different frequency bands within the infraslow range (very slow brain waves) to see if the observed changes were specific to certain speeds of brain activity.
The researchers observed that individuals with depression showed a reduced global signal correlation in their visual cortex. This means that the activity in their visual cortex was less representative of the overall brain activity compared to healthy individuals.
“The visual cortex neural activity is abnormally slow in depression: it exhibits less changes over time and thus remains more static,” Northoff told PsyPost.
The researchers also found that the visual cortex in the depressed group exhibited increased functional connectivity with several other brain regions, including the retrosplenial cortex, hippocampus, thalamus, and areas of the prefrontal cortex. This indicates that the visual cortex in depression is more strongly connected to brain areas known to be involved in emotional processing and the default mode network, a network of brain regions active during rest and self-reflection, which is often implicated in depression. These stronger connections were observed for the visual cortex as a whole, as well as for the specific regions V1 and hMT+.
“I suspected that the visual cortex neural activity would be too slow as based on earlier findings and subjects’ reports/experience of too slow visual perception,” Northoff said. “But I was surprised that the abnormal slowness was so widespread and pervasively relayed to other regions in the brain – the whole brain seems to be too slow in depression showing less changes over time in its neural activity: this relates well to exactly the same kind of experiences in the patients that nothing changes at all.”
When examining different frequency bands, the researchers found that the reduced global signal correlation in the visual cortex of depressed individuals was most pronounced in the faster end of the infraslow frequency range. In other words, the part of the brain’s signal that normally would show more dynamic, faster variations was especially reduced in the depressed individuals.
Most strikingly, the study found a significant negative correlation between the median frequency in the visual cortex and depression symptom severity. This means that individuals with slower brain activity in their visual cortex tended to have more severe depressive symptoms overall, and specifically more pronounced psychomotor retardation.
The researchers acknowledge some limitations to their study. Because they used resting-state fMRI, they could only examine spontaneous brain activity and could not directly assess how the visual cortex responds to visual stimuli. Furthermore, functional connectivity analyses can only show associations between brain regions, not cause-and-effect relationships. It is also important to note that the patient group was taking medication, which could potentially influence brain activity, although the researchers did consider medication load in their analysis and found it did not change the results.
Future research could investigate how the visual cortex in depression responds to actual visual stimuli, particularly fast-changing ones, to see if the observed slowness in spontaneous activity translates to impaired visual processing. Studies could also employ techniques that can establish causality, such as transcranial magnetic stimulation, to explore whether altering visual cortex activity can directly impact depressive symptoms.
Long-term, the researchers hope that their findings can contribute to the development of brain-based markers for depression that could aid in diagnosis and treatment monitoring, and potentially guide the development of more targeted therapies.
The study, “Abnormally slow dynamics in occipital cortex of depression,” was authored by Andrea Scalabrini, Sara Poletti, Benedetta Vai, Marco Paolini, Yuan Gao, Yu-Ting Hu, Dong-Yu Liu, Xue Mei Song, Zhong-Lin Tan, Clara Mucci, Cristina Colombo, Francesco Benedetti, and Georg Northoff.