A new study published in Nature Neuroscience has uncovered an important role for a specific type of brain cell, called oligodendrocytes, in the formation of amyloid plaques—a hallmark of Alzheimer’s disease. These cells, previously thought to be unrelated to plaque buildup, were found to contribute to about 30% of the amyloid plaques in mouse models of Alzheimer’s, with the rest produced by neurons.
The study’s findings challenge the traditional understanding that neurons are the primary source of these plaques and could open the door to new treatment strategies that target both neurons and oligodendrocytes.
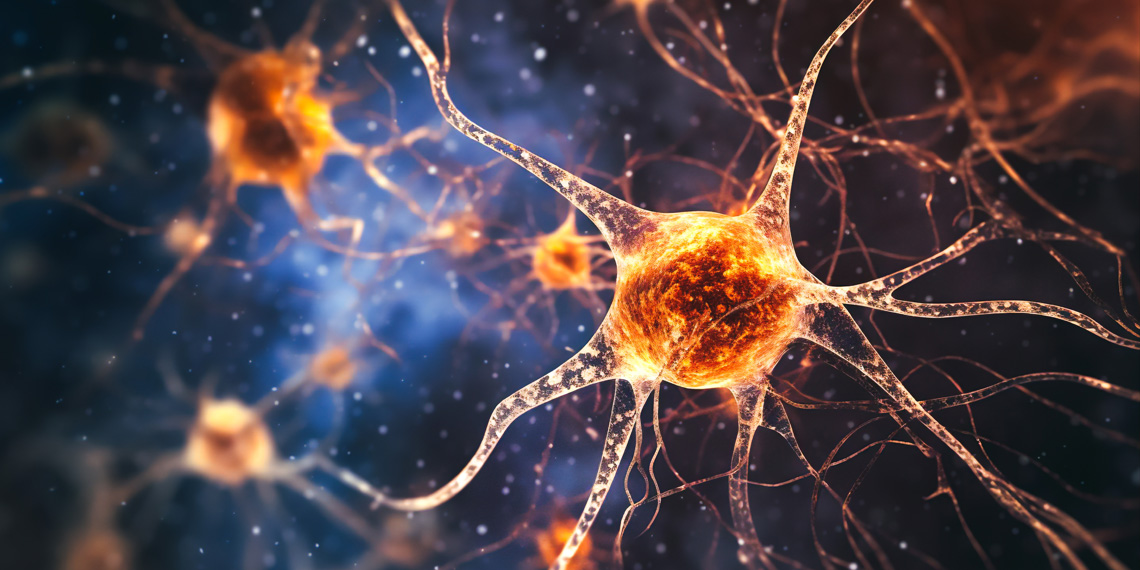
Alzheimer’s disease affects millions of people worldwide, yet its underlying causes remain poorly understood. One of the primary features of Alzheimer’s is the buildup of amyloid-beta plaques in the brain, which are thought to disrupt communication between neurons and lead to cognitive decline. Traditionally, neurons have been identified as the sole producers of amyloid-beta proteins that form these plaques.
However, previous studies have hinted that neurons might not be the only source of amyloid-beta. This new study was designed to explore whether other brain cells, specifically oligodendrocytes, could also contribute to plaque formation. Oligodendrocytes are glial cells that form myelin, the insulating layer that helps neurons send electrical signals efficiently. Investigating their role in amyloid production could provide a broader understanding of Alzheimer’s disease and point to novel therapeutic approaches.
“Alzheimer’s disease is a debilitating neurodegenerative disease and the leading cause of dementia. Although some therapeutic options exist to mitigate disease symptoms, and some are targeted and approved as therapies, most have limited effects and only delay disease progression slightly. Moreover, no preventative measures exist against Alzheimer’s disease, which is expected to be more prevalent in our aging population,” said corresponding author Andrew Octavian Sasmita, a postdoctoral researcher at University College Cork.
“The exact cause of Alzheimer’s disease remains debated and is still generally unknown, but disease hallmarks include the accumulation of amyloid-beta plaques and hyperphosphorylated tau neurofibrillary tangles. The former is known to deposit earlier and influences the aggregation of the latter. Although viewed as pathological deposits, both proteins are generated intrinsically by our neural cells, and it remains a question whether the disease progresses due to the overproduction or failure of clearance of such proteins.”
“Most available therapies have been aimed at targeting amyloid-beta, including the recently approved amyloid-beta immunotherapy,” Sasmita explained. “However, the cellular source of amyloid-beta itself has remained debated, especially in recent years, with past research acknowledging that neurons, especially excitatory neurons, are the sole producers of amyloid-beta that get deposited into plaques. Our study sought to fill in this research gap and to answer the question of whether other cell types in the brain contribute to amyloid-beta deposition, which is a key concept in our basic understanding of Alzheimer’s disease.”
The researchers conducted the study using genetically modified mice designed to model Alzheimer’s disease. These mice carried specific mutations that caused their brains to produce amyloid-beta plaques. To investigate the role of oligodendrocytes in plaque formation, the scientists employed a method called RNA sequencing, which allowed them to analyze gene expression in different cell types within the brain. They focused on a protein called BACE1, which is a key enzyme in the production of amyloid-beta.
In the first part of the experiment, the team selectively “knocked out” BACE1 production in oligodendrocytes, meaning they disabled the gene responsible for creating BACE1 in these cells. By doing this, the researchers could measure how much less amyloid-beta was produced when oligodendrocytes were unable to produce BACE1. They then compared these findings to a second group of mice in which BACE1 was knocked out only in neurons. The researchers were able to measure the resulting changes in plaque formation in both groups of mice.
To quantify the amount of amyloid plaque, the researchers used a combination of molecular imaging techniques and biochemical assays. These methods allowed them to visualize the plaques in the brain and measure amyloid-beta levels, providing a clear comparison between mice with functioning BACE1 in oligodendrocytes and neurons and those without.
The researchers found that when BACE1 was knocked out in oligodendrocytes, the amount of amyloid-beta plaques in the brain was reduced by about 30%. This means that nearly one-third of the amyloid plaques found in the brains of Alzheimer’s model mice were produced by oligodendrocytes.
These findings were surprising because previous research had focused almost exclusively on neurons as the producers of amyloid. “However, we discovered that amyloid processing components are expressed by various neural cell types, particularly oligodendrocytes,” Sasmita told PsyPost.
In contrast, when BACE1 was knocked out in neurons, the researchers observed a much larger reduction in amyloid plaque formation. This confirmed that neurons are still the primary contributors to amyloid plaque buildup, but the significant role played by oligodendrocytes suggests that they also make an important contribution, especially once plaque formation has started.
According to Robert Vassar, one of the study’s co-authors and a professor at Northwestern University, neurons seem to “get the ball rolling” in terms of amyloid plaque buildup, but once a certain threshold is reached, oligodendrocytes become a major contributor to further plaque accumulation.
“By combining various findings from our study, we highlighted that the production of amyloid-beta itself does not linearly correlate with amyloid plaque deposition, the latter being the most well-known readout of Alzheimer’s disease mouse models in preclinical research,” Sasmita said.
“Simply put, a certain percentage reduction in amyloid plaque pathology due to any intervention does not mean that amyloid-beta production is halted by that same percentage. In fact, it is less than the said percentage amount. This is due to the non-linear relationship between amyloid-beta production and plaque deposition, which follows sigmoidal kinetics. Amyloid-beta molecules need to reach a certain threshold concentration in the brain before plaque deposition occurs. This is an often-overlooked concept in Alzheimer’s disease.”
The researchers also noted that amyloid produced by neurons in the cortex and hippocampus could travel along neuronal projections and deposit in other brain regions, indicating that amyloid plaques can form not only locally but also distally via long neuronal connections.
“In one arm of our study, we ablated BACE1 in excitatory neurons primarily in the cortex and hippocampus,” Sasmita said. “However, this resulted in not only a major reduction of local plaque numbers but also distal ones in deeper, subcortical regions, such as the thalamus. This indicates that neuronal amyloid-beta is released to form extracellular plaques via long neuronal projections (axons) and also at synaptic terminals.”
The new finding that oligodendrocytes play a significant role in amyloid plaque formation could help explain why many current therapies targeting neurons have not been as effective as hoped.
“Selectively targeting amyloid processing components in oligodendrocytes could prove beneficial,” Sasmita said. “In fact, BACE1 inhibitor clinical trials failed due to, presumably, the detrimental effects of widespread BACE1 inhibition, especially on neuronal well-being. Further basic research is required, however, to better understand the functions of amyloid processing in non-neuronal cells, especially oligodendrocytes. This is imperative before moving further in leveraging non-neuronal amyloid processing for disease therapies.”
As groundbreaking as these findings are, the study has some limitations that need to be considered. First, the research was conducted in mouse models of Alzheimer’s disease, which, while informative, do not perfectly replicate the human condition. The role of oligodendrocytes in human brains may differ from what was observed in mice. Oligodendrocytes are also more abundant in humans than in mice, so their contribution to amyloid plaque formation could be even greater in people with Alzheimer’s disease.
“A recent study (Shapson-Coe et al., 2024) showed that oligodendrocytes are the predominant cell type in a human cortical region, which implies that non-neuronal amyloid-beta production could differ largely between mouse models and patients, especially given that mice have far fewer oligodendrocytes and white matter,” Sasmita noted.
Another limitation is that the study only looked at the effects of BACE1 knockout at a specific point in the disease process. It is unclear whether targeting BACE1 in oligodendrocytes later in the disease would produce the same reduction in amyloid plaques or if early intervention is necessary for this approach to be effective.
“Although this study has limited immediate clinical relevance, it furthers our knowledge on the basic pathophysiology of Alzheimer’s disease and opens up alternative avenues for therapeutic strategies,” Sasmita said.
Future research could explore several important questions raised by this study. For example, researchers could investigate whether targeting BACE1 specifically in oligodendrocytes could lead to effective treatments for Alzheimer’s disease in humans. Another promising area for future research is to explore whether other types of brain cells contribute to amyloid-beta production. While this study focused on oligodendrocytes, other glial cells such as astrocytes and microglia might also play a role in plaque formation.
The study, “Oligodendrocytes produce amyloid-β and contribute to plaque formation alongside neurons in Alzheimer’s disease model mice,” was authored by Andrew Octavian Sasmita, Constanze Depp, Taisiia Nazarenko, Ting Sun, Sophie B. Siems, Erinne Cherisse Ong, Yakum B. Nkeh, Carolin Böhler, Xuan Yu, Bastian Bues, Lisa Evangelista, Shuying Mao, Barbara Morgado, Zoe Wu, Torben Ruhwedel, Swati Subramanian, Friederike Börensen, Katharina Overhoff, Lena Spieth, Stefan A. Berghoff, Katherine Rose Sadleir, Robert Vassar, Simone Eggert, Sandra Goebbels, Takashi Saito, Takaomi Saido, Gesine Saher, Wiebke Möbius, Gonçalo Castelo-Branco, Hans-Wolfgang Klafki, Oliver Wirths, Jens Wiltfang, Sarah Jäkel, Riqiang Yan, and Klaus-Armin Nave.